Claim Management Agent with fraud detection
Claim management and fraud detection for insurance companies
A Claim Management Agent automates the entire claim management process and recognizes suspicious claims with its integrated fraud detection feature. It is fast, accurate, and provides full justification for its conclusions.
Intelligent claims management and fraud detection in seconds
Fraud costs insurers huge sums every year. An AI-supported Claim Management Agent recognizes suspicious claims as they are reported and so reduces fraud costs.
Equipped with deep learning, anomaly detection, deepfake analysis, and multimodal foundation models, the Agent checks every report for plausibility—from image analysis and geo-checks to cost estimates—always providing transparent reasoning. The result: efficient support for claims handlers throughout the entire claim management process and a powerful protective shield against fraud that detects substantially more suspicious claims than conventional systems.
Benefits for insurers
Reliable fraud detection
Cost reduction through speed
Support for existing processes
Locally developed, locally operated
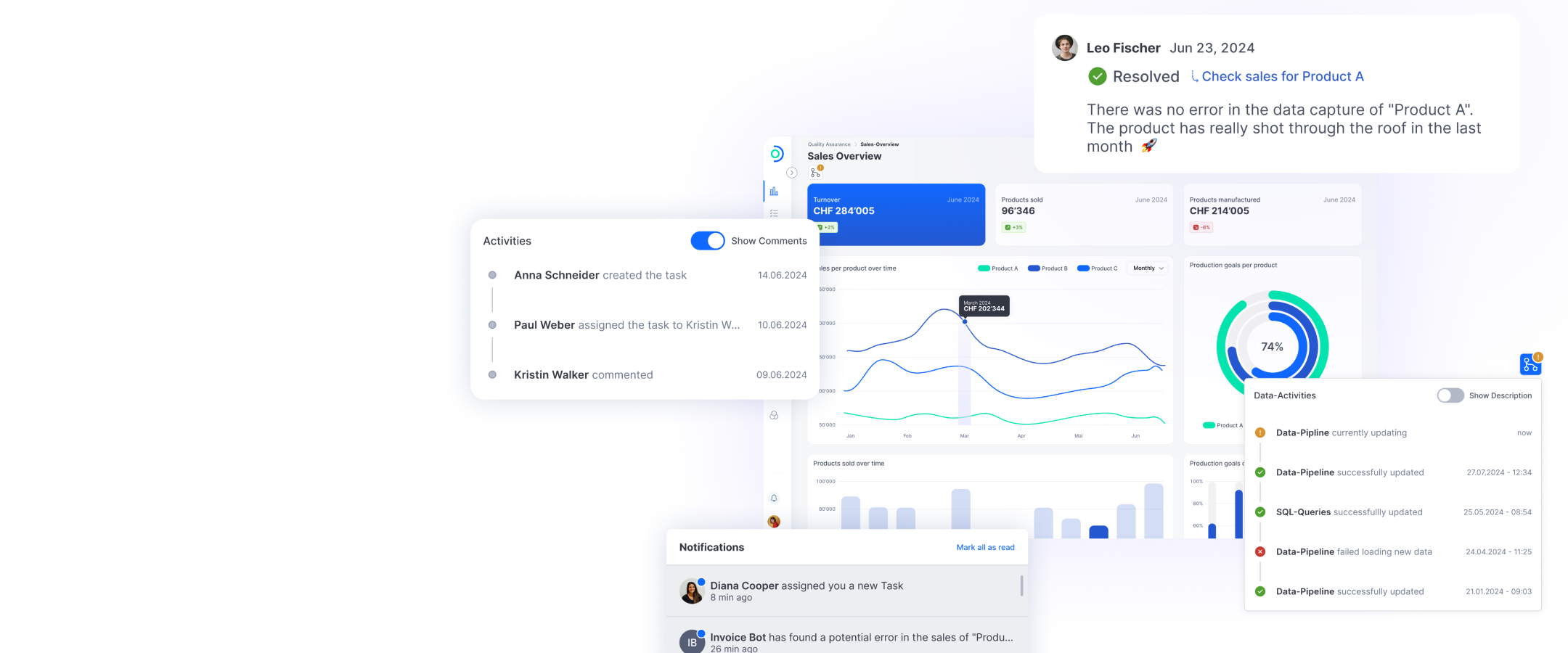
This is how a Claim Management Agent can operate

Head of AI & Digital Solutions
Lisa Kondratieva
Detect fraud faster, streamline operations, and cut costs—with AI that adapts to your insurance company’s specific needs.